This nursing care plan for pain focuses on the assessment and management of acute Pain in the hospital or home care setting.
Definition of pain:
A generally unpleasant emotional and sensory experience that occurs in response to actual or potential tissue trauma or inflammation Referred to as the fifth vital sign.
Types of pain
Acute pain:
Mild to severe pain lasting less than 6 months; usually associated with a specific injury; associated with a sympathetic nervous system response; results in increased pulse rate and volume, increased respiratory rate and depth, increased blood pressure, and increased glucose levels; urine production and peristalsis decrease.
Acute pain has a protective function to alert the patient to injury or illness. The sudden onset of acute pain prompts the patient to seek relief. The physiological manifestations that occur with acute pain result from the body’s response to pain as a stressor. The patient’s cultural background, emotions, and psychological or spiritual distress may contribute to suffering from acute pain. Pain assessment can be difficult, especially in older patients in whom cognitive impairment and sensory perception deficits are more common.
Chronic pain:
Mild to severe pain lasting longer than 6 months; associated with the parasympathetic nervous system; the patient may not exhibit signs and symptoms associated with acute pain; may lead to depression and decreased functional status
Terms used for pain
- Pain threshold: minimum amount of stimulus required to elicit a sensation of pain
- Pain tolerance: the maximum amount of pain a patient is willing or able to tolerate
- Reference pain: pain felt in an area other than the site of tissue trauma
- Untreatable pain: pain that cannot be relieved by conventional treatments
- Neuropathic pain: pain caused by a neurological disorder and not necessarily associated with tissue damage
- Phantom pain: pain that is felt in a missing part of the body
- Radiating pain: pain felt at the source of pain that spreads to other areas.
Nursing Care plan for pain with intervention and pain
Pain associated with
- medical problems
- Diagnostic procedures and medical treatment
- Traumatic
- Emotional, psychological
- Aspirational
- Cultural suffering.
Desired Outcomes
- Patient reports satisfactory pain control with a score of less than 3 to 4 on a rating scale of 0 to 10
- Patient is able to use pharmacologic and nonpharmacologic pain relief strategies.
- Patient feels more comfortable, such as controlling pulse, blood pressure, breathing, and relaxed muscle tension and posture.
May be characterized by.
- Protective behavior, protection of the body, self-centered, narrowed focus
- Relief or distraction behavior
- Facial mask of pain
- Attention in muscle tone
Below the table of Nursing care plan for pain with intervention and rationale
| Nursing intervention | Rationale |
| Assessment of pain characteristics. ex. Quality, severity, location, onset, duration, precipitating and relieving factors | Assessment of the pain experience is the first step in planning pain management strategies. The patient is the most reliable source of information about his or her pain. |
| Screening for signs and symptoms related to pain. | Some people deny the sensation of pain even though it is present. Paying attention to signs associated with pain can help the nurse assess pain. A patient with acute pain may have elevated blood pressure, heart rate, temperature, be agitated, and have difficulty concentrating. |
| For scientific findings and symptoms associated with chronic pain, such as fatigue, decreased appetite, weight loss, change in posture, disruption of sleep patterns, anxiety, agitation, or depression. | Patients with chronic pain may not exhibit the physical changes and behaviors associated with acute pain. Pulse and blood pressure are usually within the normal range. |
| Evaluate the patient’s response to pain and pain management strategies. | It is important to assist the patient in presenting the effect of pain-relieving measures as factually as possible. Discrepancies between the patient’s behavior or demeanor and what he or she says about pain relief. |
| Assess patient’s expectations for pain relief. | Some patients are satisfied with pain relief, while others expect complete elimination of pain, which affects their perception of the effectiveness of the treatment method and their willingness to participate in further treatment. |
| Anticipate the need for pain relief. | The most effective way to address pain is to prevent it. Early intervention can reduce the total amount of analgesics needed. |
| Eliminate additional stressors or discomfort whenever possible. | Patients may experience exaggeration of pain or diminished ability to tolerate painful stimuli if they experience additional stress from environmental, intrapersonal, or intrapsychic factors. |
| Provide rest periods to promote comfort, sleep, and relaxation. | The patient’s perception of pain may be exaggerated by fatigue. In a cycle, pain can lead to fatigue, which in turn can lead to exaggerated pain and fatigue. A quiet environment, a darkened room, and a phone turned off are measures that facilitate recovery. |
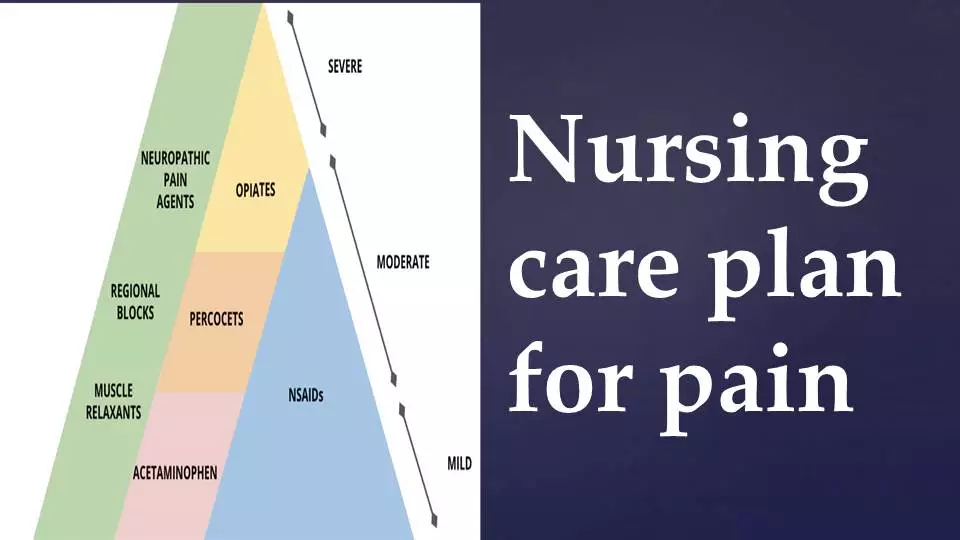
| Determine the appropriate method for pain relief. | Unless contraindicated, all patients with acute pain should receive a nonopioid analgesic around the clock. |
| Hot or cold compress | Heat reduces pain by improving blood flow to the area and reducing pain reflexes. Cold reduces pain, inflammation, and spastic massage by decreasing the release of pain-inducing chemicals and slowing the transmission of pain impulses. |
| Massage of the painful area | Increases endorphin levels and decreases tissue edema. This intervention may require another person to perform the massage. |
| Administer analgesics as ordered by a physician, evaluate their effectiveness, and observe signs and symptoms of side effects. | Analgesics are absorbed and metabolized differently by patients, so their effectiveness must be assessed by the patient individually. Analgesics usually have side effects that range from mild to life-threatening. |
| Notify the physician if interventions are unsuccessful or if current symptoms represent a marked change from the patient’s previous pain experience. | Patients who request pain medications at shorter intervals than prescribed may actually require a higher dose or stronger analgesics. |
| Anticipatory education about the causes of pain and appropriate measures for prevention and relief. | Knowing what to expect can help patients develop effective coping strategies for pain management. Patients need to learn the importance of reporting pain early to achieve more effective pain relief. |
| The patient should learn how to effectively discontinue the medication dose in relation to potentially unpleasant activities and avoidance of pain spikes. | Patients must learn to use pain relief strategies to minimize the pain experience. |
| Assist the patient and family in identifying lifestyle changes that can contribute to effective pain management. Guide the patient to plan activities during the times when pain is at its greatest relief. | Changes in work routine, household responsibilities, and home environment may be necessary to promote more effective pain management. Ongoing support and guidance for the patient and family will increase the success of these strategies. |